Medicaid Emergency Room Copay

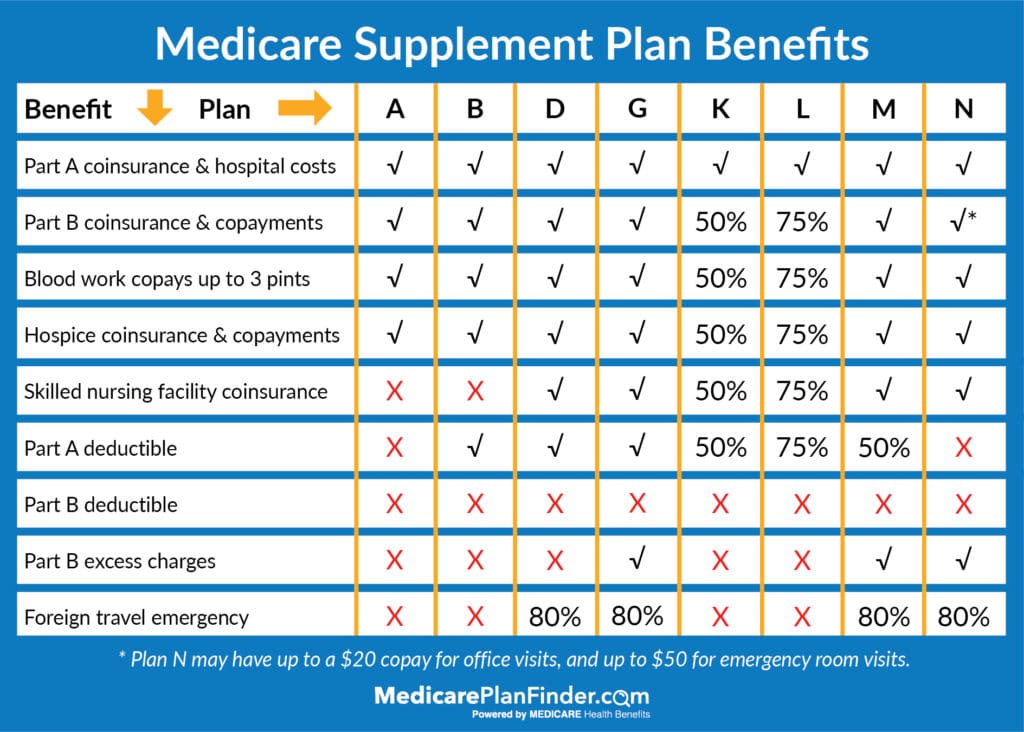
You also pay 20 of the medicare approved amount for your doctor s services and the part b deductible glossary applies.
Medicaid emergency room copay. When a medicare recipient requires emergency care medicare does cover emergency room visits for the most part and the recipient pays a copayment. There is a monthly co pay maximum for health first colorado members. If you re admitted to the same hospital for a related condition within 3 days of your emergency department visit you don t pay the copayment because your visit is considered. Cost sharing for most services is limited to nominal or minimal amounts.
In washington state medicaid is called apple health. If you qualify for mississippi medicaid health benefits some medical services may require a copay small fee. Children under the age of 18. However you may have to pay a small co pay for other benefits such as certain lab tests medical supplies and emergency room visits.
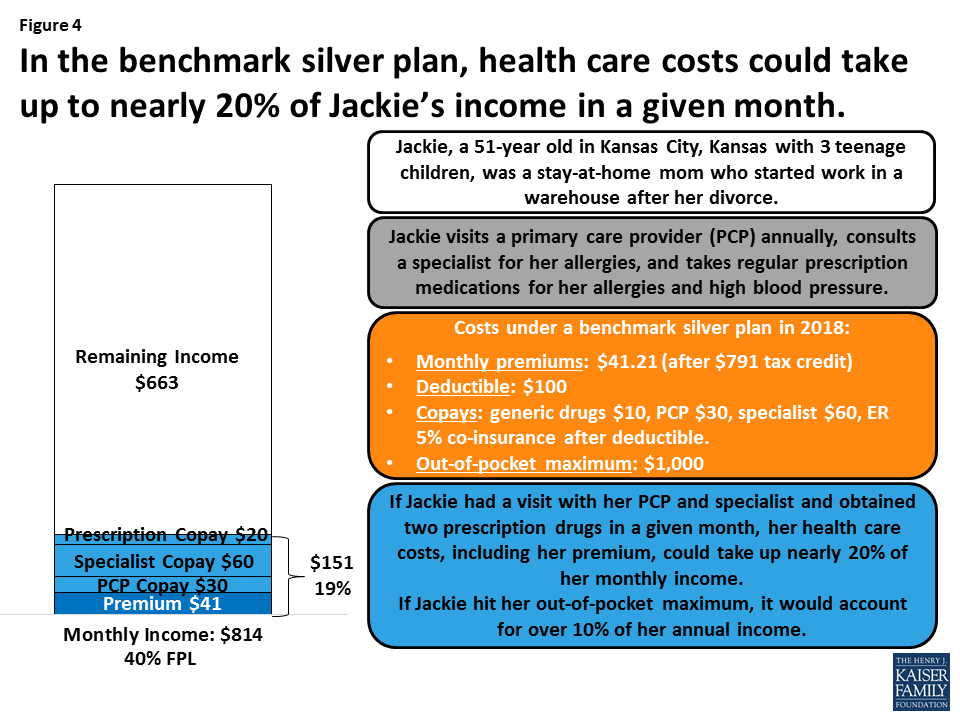
The maximum copayment that medicaid may charge is based on what the state pays for that service as described in the following table. Copays are not required from these groups of people. Individuals in nursing homes or facilities. And if you live in new york you will be covered for all required federal benefits.
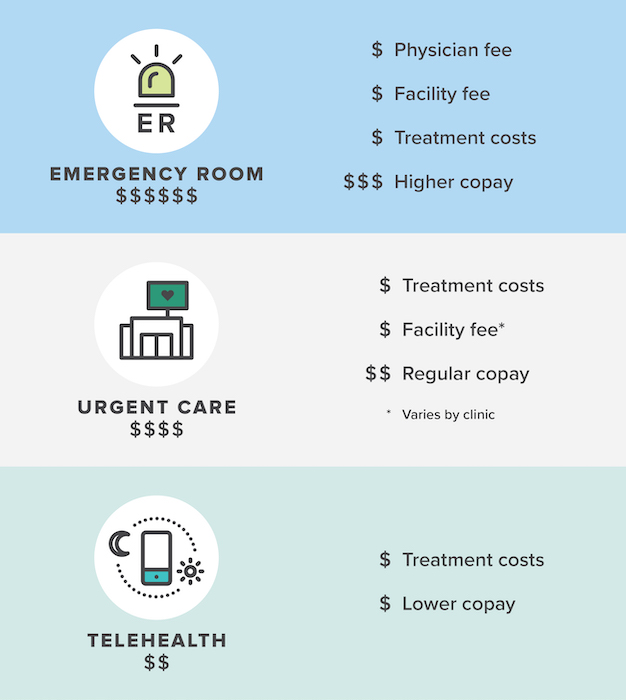
For patients covered by health insurance out of pocket cost for an emergency room visit typically consists of a copay usually 50 150 or more which often is waived if the patient is admitted to the hospital depending on the plan costs might include coinsurance of 10 to 50. Read on to learn more about emergency room costs and how a medicare supplement insurance plan can help reduce what you pay out of pocket for. Or you might not be sure if it s an emergency and visit the er to be on the safe side. States are required to provide the following mandatory medicaid benefits under federal law.
Medicaid copay for emergency room er visits. You pay a copayment for each emergency department visit and a copayment for each hospital service. Emergency services are exempt from medicaid copay. Emergency services in an.
If you are a biller provider or partner. This means once a member has paid up to a certain amount in co pays in a month they don t have to pay any more co pays for the rest of that month. In addition medicaid enrollees may be denied services for nonpayment of alternative copayments. But there are situations and reasons why you may visit the er even when it is not an emergency.
5 of the member s monthly household income. You will get the same result for a smaller copay. This maximum is based on a formula. Original medicare is a federal health insurance program for seniors and people with certain disabilities.
Maximum nominal out of pocket costs. This means that an insured person would need to meet their annual deductible of 198 before medicare pays for emergency room er visits. An emergency room visit typically is covered by health insurance. Copays are not required for these services.